In Part One of my discussion of Robert Whitaker’s Anatomy of an Epidemic, we learned that there is no scientific basis for the theory that mental illness results from an imbalance in brain chemistry; Part Two showed how, in the main, patients who were never given psychiatric meds have far better outcomes than people exposed early on to such drugs. In this third and final part, I’ll discuss what these medications actually do to your brain chemistry and why they lead to a worse prognosis in the long run.
In order to understand these processes, we need a bit of basic neurology. I’ll try to keep it simple. As you probably know, the brain is made up of billions of neurons; each one of these neurons is connected to many other neurons. Messages travel along the neurons, to and from the brain, moving from one neuron to another across a tiny gap called a neural synapse or the synaptic cleft. One neuron releases a chemical messenger called a neurotransmitter into the synapse; the molecule then travels across that tiny gap and bonds to the next neuron on the other side, thereby delivering its message. The message subsequently continues along this second neuron until the next synapse, and so on. Here’s a diagram of a typical neural synapse; you can ignore most of the labels:
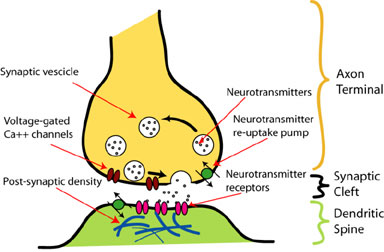
So the message travels down the yellow neuron, releasing neurotransmitters into the synaptic cleft. On the other side, the green neuron has receptors (the red ovals) where the neurotransmitter bonds, thereby sending a message which then travels down the green neuron to the next synapse, and so on. After the message has been sent, the neurotransmitter is released from the receptor back into the synapse where one of two things occurs: either another chemical agent, an enzyme, goes to work on the neurotransmitter and dissolves it, or the (yellow) neuron re-absorbs it for later use.
Dopamine and serotonin are two neurotransmitters that have been implicated in mental illness, dopamine for schizophrenia and serotonin for depression.  The low-serotonin theory of depression (which, as I discussed in Part One, has no basis in scientific fact) holds that depression results from low levels of serotonin within the brain — i.e., not enough of those serotonin molecules delivering the message across the synaptic cleft.  An insufficient amount of delivered serotonin messages theoretically makes you depressed. By either increasing the amount of serotonin, or making the lower levels more effective, we will theoretically correct the chemical imbalance and alleviate your depression.
The drugs known as the “selective serotonin reuptake inhibitors” (SSRIs) (of which Prozac, Zoloft, Paxil, etc. are members) have been sold as correcting this imbalance by the second of those methods. By preventing the first (yellow) neuron from re-absorbing serotonin and instead leaving it within the synapse, that neurotransmitter can continue to act as a chemical messenger and dock repeatedly with the post-synaptic (green) neuron. So in theory, instead of having the “normal” amount of serotonin molecules acting only once and then being reabsorbed, you would have a lower-than-normal amount of serotonin molecules communicating more than once apiece.  If the brain needs, say, 100 serotonin messages sent, it theoretically makes no difference if you have 100 serotonin molecules each delivering one message, or 50 serotonin molecules delivering the message twice. I hope that makes sense.
There is ample scientific evidence that SSRIs do exactly that, they interfere with the re-absorption of serotonin by the pre-synaptic (yellow) neuron, allowing the neurotransmitter to deliver its message repeatedly. For about a third of the people who take an SSRI, this leads to a temporary improvement in depressive symptoms even though we know that they did not have reduced levels of serotonin (and this improvement is no better than for those individuals given a placebo). On the contrary, there were normal levels of serotonin before the introduction of the drug, so an SSRI has the effect of boosting serotonin levels in the synapse to above-normal.
Because the body believes there is now too much serotonin, more than it needs, it disables some of those docking spots (receptors) on the post-synaptic (green) neuron because it doesn’t need so many, thus reducing the number of serotonin messages it receives. In other words, too much serotonin leads to fewer receptors for receiving the chemical message. So not only do SSRIs introduce a chemical imbalance where none existed before, they cause the body to modify itself in order to address that imbalance.
What happens if you then remove the drug from the system? As re-absorption levels revert to normal, Serotonin levels within the synapse drop dramatically, but you have fewer receptors to receive the messages. This can be a psychological disaster, as many people will testify, and the body now needs those drugs in order to re-establish this new unnatural chemical “balance”. Paradoxically, this has convinced many physicians and patients that the drugs are “working”: after all, if you do much worse without the drugs, doesn’t that mean they were having a beneficial effect? The far more troubling answer is no, the drugs have altered your brain chemistry so that you experience withdrawal symtoms without them. It’s as if the pharmaceutical industry, in association with the American Psychiatric Association, has created a giant new group of drug addicts.
The way that the brain adapts to an artificially introduced chemical imbalance is the same for other classes of drugs: the anti-psychotics, benzodiazepines, stimulants used to treat ADHD, etc.  It helps to explain why, despite what we hear over and over, that taking these miracle drugs restores balance to your brain chemistry (just as insulin addresses a chemical deficit in diabetes), mental health outcomes are worsening and disability due to mental illness is skyrocketing.
Whitaker does not argue that psychotropic medications have no place in the treatment of mental illness; he believes these drugs may be useful for stabilizing psychotic patients and in short-term use for other disorders. But the widespread prescription of these drugs for long-term use has been an unmitigated disaster, for millions of individuals and for our country as a whole.
Given that some people appear to be helped by SSRIs, it seems likely that serotonin plays an unspecifiied role in depression; however, by preventing the re-absorption of serotonin, SSRIs affect every neuron within the body that uses it to send messages and therefore alter the entire neural system — hence all those nasty side effects. As much as the APA and pharmaceutical industry would like to believe we’ve made great scientific strides and can now produce drugs that rectify specific chemical imbalances for specific mental disorders, thereby effecting a “cure”, it’s simply not true.
Finding Your Own Way:
There’s a wealth of material in The Anatomy of an Epidemic, much more than I can do justice to. Please read Whitaker’s book. If you’re like me, the experience will be unforgettable.
45 thoughts on ““Psychiatric Meds Are Like Insulin for Diabetes” (Big Lie #3)”
Wow, that is frightening. And, I imagine that it will not be perhaps for another 20 years that we will see the longterm affects of these drugs on human beings. I ‘shudder’ when I acknowledge that 5 out of my 8 immediate family members take these drugs – as they say, their ‘happy’ drugs. I feel sad that they have not been able to face what it is that ‘made’ them feel depressed in the first place. But, this is the world we live in – one of masking pain, buying more and more ‘things’ and being crazy busy – all ways of avoiding reality.
Yes We Do. I just got the drug from a firend thank g-d I came cacross this maitrial .. I know it but never belived it was ture untill I read it from you guys. thanks!!
As unsettling as this blog has been I appreciated reading what you had to say. I just ordered the book. I think it is important information and I am glad you shared it. The biggest hook for these drugs is that initially they provide some relief and then people end up staying on them for a lifetime doing the “SSRI dance” from one type to another. I have always been reluctant to refer people to doctors for drug therapy. We live in a society that wants quick results and the drugs provide that for some. Therapy takes time and people may not see results as quickly. Again, thanks for your providing us with your thoughts on this important topic.
Renee Segal
THOT-PROVOKING AS EVER, YOU ARE . IT’S SURE TRUE THAT THE DRUG COMPANYS’ ” RESEARCH” IS WOEFULLY UN-SCIENTIFIC ( THO SADLY , MAINSTREAM “SCIENCE” ALSO STRONGLY RESISTS PUBLISHING , & FUNDING-AGENCIES ALSO ESCHEW NEGATIVE RESULTS). AS WELL AS GROSSLY MIS-INTERPRETED BY THEM & THEIR DAMN REPS ( IN THEIR OWN INTERESTS ). iT’S ALSO TRUE THAT , MOST OF THE BEDROCK ,
FUNDAMENTAL EFFECTS FOUND & MOST QUOTED & ACCECPTED IN ALL HARD & SOFT SCIENTIFIC FIELDS HAS NOT BEEN WELL-REPLICATED , IF REPLICATED AT ALL. aND WHEN IT HAS BEEN WELL REPLICATED , A HORRORIFYING “DIMINISHING EFFECT ” HAS BEEN RECENTLY DEMONSTRATED IN OVER 1/2 OF THOSE BASIC STUDIES, WHICH INCREASES W/ EACH REPLICATION . THIS LEAVES US TO MARVEL AT THE ACTUAL HIGH ! & CONFOUNDING OCCURANCE OF STATISTICAL “IMPROBABILITY” IN THE ANALYSIS OF STUDY RESULTS. WHETHER MUCH OF ANYTHING CAN BE ESTABLISHED & BELIEVED IN SCIENCE BECOMES A VERY UN-PLEASANTLY VALID PERSPECTIVE.
bE THAT AS IT IS , MY PERSONEL & PROFESSIONAL EXPERIENCE CLEARLY SHOWS ( ANECDOTALLY ) THAT MANY OF THOSE PSYCH MEDS
WHOSE SCIENTIFIC STUDY IS SO CONFUSINGLY CONFOUNDED REALLY ! HELP LOTS ! MORE PEOPLE THAN MY EXTENSIVE STUDY & USE OF “PLACEBO” ( = MIND-BODY INTERACTION , IN HYPNOTHERAPY, FOR INSTANCE ) CAN EXPLAIN OR UNDERSTAND. aT LEAST WE KNOW HOW , OFTEN , WE CAN GET THESE + EFFECTS TO HAPPEN.
SO I’M LEFT W/ RESPECT & ADMIRATION FOR THE EXCEPTIONAL , FEW ! MEDICAL SPECIALISTS WHO THOTFULY , ARTFULY & PERSISTENTLY DO HELP MANY FOLKS W/ THOSE DAMN PSYCH MEDS. WE CAN VERY OFTEN HELP CLIENTS USE PSYCHOTHERAPY TO MOVE WELL BEYOND THE MED’S EFFECTS , & REGULARLY, I’VE SEEN FOLKS WHO WERE IN- ACCESSIBLE IN PSYCHOTHERAPY BECOME ! WAY BETTER & ACCESSIBLE TO PSYCHOLOGICAL APPROACHES THAN W/O MEDS. DR BOB
Can you interact at all with some of the critical reviews of the book? That the author cherry picks studies, and has no scientific background?
Greg, if you have some data you’d like to put forward, I’ll be glad to post it. I’d be particularly interested in anything you have that counters his “cherry-picking,” as you call it. At the moment, I’m continuing to educate myself and am immersed in “Prozac Backlash” by Joseph Glenmullen, M.D. He goes into greater depth than Whitaker about the long-term side-effects of SSRIs and I’ll be writing about it sometime soon. For me, this book has been another enormous shock.
I was thinking of, for example, the critical review at Boston Globe:
http://www.boston.com/ae/books/articles/2010/04/14/tying_the_rise_in_mental_illness_to_drugs_used_in_its_treatment/
Unfortunately, it’s pay to view now …
Greg, give me some time and I’ll check it out, even if it is pay-to-view. I took a quick look around the Google universe and found nothing that takes substantive issue with his methodology. I’m sure it exists, I just haven’t found it. As for Whitaker not being a physician, I think that is irrelevant. What is needed is someone who understands experimental design and statistical analysis, since the book is in part a critique of biased studies designed by the pharmaceutical companies and bogus results based on manipulation of variables and statistics.
I think there was some critique/response to his points at Alternatives conference and after his Harvard speech at Grand Rounds which should be on YouTube. I’m glad you put this information out there, but it honestly becomes confusing when different mental health professionals seem to be at odds with each other and you don’t know who to believe.
I’ll check it out. Thanks.
Joseph, what is your opinion on using MAOIs instead of SSRIs?
Suppose that the person is able to maintain a good diet while using MAOIs. Wouldn’t MAOIs be a far more superior type of drug in the long run compared to SSRIs?
Martin, I’ve had virtually no experience with MAOIs myself, but according to the long-term outcome studies that Whitaker looks at, MAOIs are no more effective than the tricylics or SSRIs. He cites two studies, one by the British Medical Counsel in 1965, which found that MAOIs were “singularly unsuccessful” in treating depression; and a review by the NIMH in 1969, more of a meta-analysis of other anti-depressant studies, that concluded, “The differences between the effectiveness of antidepressant drugs and placebo are not impressive.” These citations occur in a section on the history of anti-depressant research; there may very well be more recent studies with different outcomes.
Thanks for your reply Joseph.
I find it quite interesting that most psychiatrists have very little experience with MAOIs, even though MAOIs have been around for decades and people who have tried them have said that these drugs are absolutely fantastic. A lot of people say for instance that “Nardil” has been the miracle drug for them in treating social anxiety and that no other drug has worked so well. (but only after the psychiatrist has destroyed their body with about 10 different SSRIs – leaving Nardil as the last resort).
Ever consider the damage you are inflicting on millions of people with this type of post? You may be into Scientology, which has no place in mainstream america. Shame on you! Inflicting a hopeless state of being, shameful! I am sure this has the potential to come back and haunt you.
One of the interesting sections in Whitaker’s book covers the way the pharmaceutical industry used the slur of Scientology in just the way this comment attempts to do. Serious questions were arising about the dangers of SSRIs and had begun to get coverage in the media as well as the scientific journals. Lawsuits were being filed, prescriptions for SSRIs were dropping as concern rose within the medical profession. Then Scientology came out with one of its lunatic statements about the evils of psychiatric medication. In a brilliant feat of public relations, the pharmaceutical industry was then able to link the two — crazy Scientologists with anyone who questioned the safety of psychiatric medication — thus defusing public concerns about Prozac, etc.
I’m just coming off Paxil after 8 years on the drug. Before that I was on Prozac for 8 years. Coming off Paxil has been horrific. It’s like I’m a drug addict! Even with a very slow weening process, I’m shaky, sweaty, dizzy, nauseous, and a few other unpleasant symptoms that I won’t mention here. But I just can’t go off the medication and take nothing or I will crash, so I’m going onto Wellbrutrin next. I feel like it’s a cycle of meds that will never end and I wish there was a way to end the cycle. Thanks for the information.
Jamie
@fightdepression
I think that using chemical interventions is a hack…a very blunt one. It affects the whole brain, rather than a specific region. For what it’s worth, I much prefer to respect the very complicated biochemistry of the system and use such interventions as a last resort, rather than a knee-jerk first reaction to mental distress.
Me, too. I do think that meds have their place but (as you say) as a last resort.
HELLO EVERYONE IAM JUST ABIT CONFUSED ,SO WHATS THE DIFFERENCE BETWEEN SITUATIONAL DEPRESSION AND CLINICAL DEPRESSION WHY DO THEY CALL IT CLINICAL DEPRESSION ,AND THE MOST SEVERE DEPRESSIONS ARE THEY BETTER OF WITHOUT MEDS?THANK YOU
Situational depression might be a normal response to loss, such as grieving after the death of a loved one. With time, most people recover. Clinical depression is one that doesn’t occur in response to an external event and the depressed person doesn’t recover. I feel that meds may be useful in severe cases of depression, to help people break out of a chronic state, but studies show anti-depressants have no benefit after about 6-8 weeks.
thank you very much for your answer
Hi. I`m a bit worried because I experienced a serius trauma, and contacted a psychiatrist. I was still in shock, so even though I knew how dangerous benzodiazepiner is, I was not able to protect myself. After seven weeks (I was so drugded) I managed to stand up for myself and went back to Oslo where I live and work. When I found out the extent of the amount of medication dose (100 mg Sobril per day, 7,5 mg Imovane and SSRI) I panicked . Before I met the therapist I didn`t use any medication. I managed to cut down on medication, but it was a tough journey. In addition to the initial trauma, I also strongly withdrawal. It took me one year before I was clean. I felt like an addict although I never would have voluntarily taken this. How much do you think this has effected my brain?
I’m Norwegian so sorry that my written English is not so good. We often speak better English than we write.
Best regards
I doubt there have been any lasting effects, given how short a time (comparatively) you were on those medications. Good for you that you stood up for yourself and went through the hell of benzodiazepine withdrawal.
not JUST the brain – all seratonin sites throughout your entire body.
MAO inhibitors are used routinely to treat Parkinson’s Disease. They work at an enormous cost: eventual dementia. The disease is then called Parkinson’s Plus. (Don’t expect the medical community to admit that, even though the dementia aspect of PD was unknown until the medications were widely over used.) There is a really informative web site called the Parkinson’s Recovery Project (www.pdrecovery.org), that goes into great detail about, among other things, how MAOI’s work. That web site ‘look’ has changed (for the better) since I last looked at it in depth and downloaded it’s ebook(s?) a couple of years ago, but appears to have the same plethora of interesting, logical and very controversial information. Everything I read rang true with PD progression that I observed first hand.
Medications that affect the brain are so very, very dangerous…
Thanks for that link. I’ll check it out.
Wow, this series of posts was really informative. I will definitely look at the book. I have a long history of depression and found that my problems were quite fundamental and complicated, but throughout my time struggling I did not want to take medication because it scared me. I did find that there was a lot of pressure at times to do so, particularly when my problems were interfering with school or when therapy was not going well.
I remember at one point I joined a support group for depression, and found that I was one of the few ones there not taking some form of medication. Most of the people at the support group seemed to have mixed feelings about their medications – they would tell me “SSRI’s saved my life” and then in the next breath they would go on to say that they were having trouble living without their medications. A few of them seemed to have once been creative people who told me that they did not feel inspired or in awe of the world anymore, as they once had. I was unsure at the time of whether my fear of medication was irrational, and I asked several of them if they thought I should go on antidepressants. When I told them I liked to paint and art was a big part of my life, they told me not to do it.
I’m glad I listened to them. Now I am feeling much happier after a few more years of talk therapy, but I still feel sad for those people I met who felt that their inner lives had been dimmed and mutilated by these drugs.
I’m glad you held out. As you say, there’s so much pressure to go on anti-depressants these days … and yet so many reasons not to. If you’re a creative person, the loss of inspiration and interest in order to “cure” your depression would seem way too high a price to pay.
Hi Joseph, as a regular reader of your blog, i was reading a very good article from the New York Times on depression and evolutionary psychology and though you would be interested.
http://www.nytimes.com/2010/02/28/magazine/28depression-t.html?pagewanted=1
Thanks.
Thanks for recommending that excellent article. Whatever the value of the evolutionary psychology approach, the researchers stress that depression often has a value and it’s worth going through it, rather than attempting to medicate it away. This point has been lost in the recent trend toward medicalizing mental health and treating depression as if it were a chemical imbalance.
Am feeling really discouraged and upset after reading about this. Started taking fluoxetine about six months ago, which was actually a “last resort” for me, and was feeling really encouraged that they seemed to be helping to alleviate the pain of working against my feelings, which always seem to lead me to do the “wrong” things. In other words, taking the fluoxetine helped make doing the “right” things easier for me and seemed to be improving the quality of my life. But for the past week I’ve noticed the difficult feelings starting to come back, and now reading this, I’m wondering if this is why…and now am feeling very upset and discouraged. Ultimately would rather know the truth and deal with that. But was really hoping to finally be free of the pain.
I sympathize — I think being freely of pain is an unrealistic expectation, however. You need to find better ways to cope with your pain and take care of yourself, which means psychotherapy. The hype about drugs is very appealing; we’d all like to believe we could take a pill it and will remove our pain, but it’s simply not true.
After reading more of your posts, I realize that I may have found your information just in time, in that at this point, I’ve benefitted from the short-term effects to be had from fluoxetine, and could avoid the long-term problems you’ve described if I were to start weaning myself off of it now. I will be bringing this info to my next appointment with my doctor. Thank you for the information.
Expect resistance from your doctor. The medical establishment believes in long-term maintenance regimes for these drugs.
Thanks for your reply. I only tried the AD’s after several attempts at psychotherapy, the last of which was fairly successful and lasted two years. She was relational/psychodynamic but then moved away, which is the only reason I stopped therapy. The meds have helped me to internalize and implement many of the things we realized/she suggested in the therapy. And I do not expect complete freedom from pain, am just looking for ways to do the best I can with what I have. Thank you again for your site and for your replies.
I agree with Joseph regarding the array of drugs out there, which are prescribed without further ado, usually by very busy G.P.s
There are life events (nothing to do with family of origin problems or other such) which can knock you for six, make you anxious, make you panicky. This does not mean you are depressed. I had experience of this quite a number of years ago. A lot of bad things happened, and they happened together, and it really torpedoed me. In general I would be a resilient person, but this was a serious state of affairs. Anyhow, feeling shaken, panicky, pretty exhausted, I took myself to the doctor. I explained what the circumstances were, how rough I was feeling, and guess what, out came the prescription pad! Not just one box of pills, but three! I actually went to the pharmacy and bought them. Got home, looked at the boxes, and just flung the lot in the bin. I felt so grim but I was fortunate to be recommended a very good therapist (he had no belief in the “pills”), and we got to work to help me out of what was, after all, a temporary psychological jam. I was also lucky enough to have sufficient funds to pay him, and the big problem is that the vast majority do not have money for therapy. Many don’t even have another person to talk to, or their dear ones are fed up listening to them.
It is rather sad.
Hermes
I had a very similar experience, going through a traumatically rough patch and receiving a prescription for a benzodiazepine from my GP. Sadly, it’s all too common.
HI, AGAIN DEAR JOSEPH SORRY IF MY ENGLISH WRITING IS NOT SO GOOD ,I WANTED TO ASK YOU WHY DO DEPRESSED FEELINGS ACURE AFTER A PANIC ATTACK ,THAT HAPPENS TO ME USUALLY WHEN I GET REALLY STRESSED DUE TO SOME SITUATION THAT OVERWELMS ME SOMETIMES
I GET A PANICATTACK IF A GET AN OVERLOAD OF FURSTRASION THE PANICATTACK DOSENT SCARE ME THE AFTER FEELINGS DO THEY MAKE ME FEEL ABIT FEARFUL EVERYTIME ,THANK YOU SO MUCH FOR YOUR TIME
I’m not sure why those depressed feelings come up after a panic attack. I don’t think I know enough about your experience to explain it. I’m sorry I can’t be more helpful.
This post really scares me and makes me so angry because it’s clear that many people are being harmed without knowing it, including me.I was on anti-depressants for 10 years, starting when i was 16 until 26. Throughout this time I had different levels of depression which the meds always numbed. I tried 4 therapists and they didn’t work, so i gave up and basically accepted that this was my lot in life and meds were the only option.
I’m currently off of the meds (finally) and in the worst depression of my life. I’m in psychodynamic therapy (which is a really slow process), but i just really feel like if i hadn’t been on the meds for so long, the depression wouldn’t be so bad and maybe i would have made more progress by now. I think as the article mentions, my brain chemistry has been completely altered and messed with, and i really worry that now there’s no way to get out of it but to go back on anti depressants and obviously stick with therapy. It just feels like the meds brought me 10 steps back now. What’s your advice on that? Should I avoid anti-depressants at all costs now?
Don’t go back on the anti-depressants. There are studies that link long-term use of SSDIs to permanent neurological damage, dementia and a shortened life span. Just tough it out, as hard as it may be.
I am still alive because of Prozac. Whatever you think you know, you don’t, until it changes your life.
It is the one thing – after YEARS of fabulous therapy, exercise, dietary changes, behavioural modifications- that stopped the suicidal thoughts.
Like every single thing in life, it is good for some, and not good for others.
We just took my 11 year old off of some really potent drugs, Depakote, Zyprexa and Clonidine. we were fortunate enough to find a holistic psychiatrist in Chicago to help us as no one in Our area of Michigan would. She is doing so much better and I am relieved to ave her back. Her mother was always on medication and is not doing well at all. Our psychiatrist in Michigan, even though I told her we wanted to get our child off of the medications, kept insisting that we continue to medicate. A horrible situation so we stopped seeing them. Although she has only. Even fully off for a month, we are seeing a new girl who can read again and process thoughts. Looking forward to a wonderful year.
That is so very good to hear! I usually hear the horror stories and I’m glad you managed to get her off those awful meds.
Well, I have just found this blog, and to some extent I agree – SSRIs should not be prescribed for mild to moderate depression, they should have talk therapy instead.
However, when it comes to severe depression, the kind that makes you unable to get out of bed, where you’re staring at walls, crying for hours for no reason, thinking about how much you just don’t want to live anymore… I don’t believe antidepressants are destructive if they stop someone from killing themselves, and terrifying people like that with stuff like this blog entry is not the answer. Not at all.
I grew up with bipolar disorder, but wasn’t diagnosed until I was 23 (three and a half years ago). As a child I was mostly a rapid cycler; I had no control over my emotions, so if I was feeling irritable and someone said the wrong thing, I would explode in anger, and similarly I could get into strange moods where I had no filter, so I did and said pretty much whatever came into my mind. When I came down from those moods, I often felt so much guilt and shame over the smallest things that I’d feel what can only be described as depression, but it wouldn’t last very long before my mood changed again. I did, however, experience an episode that lasted about six months when I was nine, which was pretty scary as you can probably imagine, for a 9-year-old to feel so much self-hatred that they can’t focus on their homework to the point of still be struggling with it at midnight, and crying themselves to sleep every night.
I was treated like a badly behaved child, and of course I went on to become a badly behaved teenager. I was yelled at, berated, criticised and belittled. After a summer of hypomania when I was sixteen, I crashed, and had episode after episode of depression. I never fully recovered from one episode before being hit by the next one, and my brief periods of hypomania manifested in bouts of extreme rage. My teenage years were a horror fest. Upper secondary school is mostly a blur to me; I have no idea how I got through it, but I’m pretty sure I almost didn’t. I wanted to die, most of the time. I felt absolutely worthless.
At 22, I could no longer do it. My depression was so debilitating that I couldn’t function at all anymore. Fortunately, my singing teacher at university noticed, sat me down, and told me to see a doctor. Probably wouldn’t be here now if it wasn’t for her. So I went to the doctor, broke down into tears and asked for help. This is where my experience with antidepressants begins.
I was prescribed citalopram, but I experienced some pretty bad side effects on that drug, so I was prescribed an SNRI instead after a few weeks, duloxetine, which was supposed to help me sleep as well. It didn’t help me sleep, nor did it help my mood which once again started to deteriorate, so I went back to the doctor again and asked if we could try another SSRI. She gave me sertraline, and bingo. My mood started to improve.
By the time of summer 2011, I felt pretty great, actually. I had a summer job, and newfound energy, and despite some minor episodes of irritability I was mostly happy. A few months later, however, my mood began to deteriorate again. The antidepressant simply stopped working.
The next stop was a psychiatrist’s office. After a two-hour long interview, I was diagnosed with bipolar affective disorder, and prescribed quetiapine. In hindsight, I have no idea why I was given this drug; I was on it for three years, and at first feeling nothing was an enormous relief, because my whole life I had felt EVERYTHING and I was exhausted, but after a while, feeling nothing began to take its toll. I was dulled down, and it felt like I had a concrete block in my head. My cognitive abilities were really suffering.
So I went back to the psychiatrist, explained what I was experiencing, and I was prescribed lamotrigine. Coming off quetiapine was absolutely awful, my discontinuation symptoms were pretty bad, but six months later I feel so much better. No, medication is not a miracle cure, but they have provided me with a life I never knew existed. My whole life had been an endless stream of misery, so imagine what it has been like to discover that it wasn’t supposed to be like that! Medication has done so much for me; they have also provided me with enough emotional stability to start therapy, which I have been doing now for almost two and a half years.
I am able to tolerate life nowadays, and I have sertraline and lamotrigine to thank for that. I would rather be on these meds for the rest of my life, than feel the way I felt for the first 22 years of it.
I DO agree that SSRIs are prescribed far too often, though, and that prescriptions are flying all over the place to people who shouldn’t be receiving them; basically, SSRIs are being abused as some sort of “easy solution”, and this is very problematic for several reasons, one of them being that SSRIs are getting a bad rep. People left and right are complaining about how the SSRIs made them feel flat. Well, what did you expect? They aren’t actually “happy pills”! If feeling flat wasn’t a GREAT BIG RELIEF to you, you probably shouldn’t have been put on those meds to begin with. Get off them immediately!
As for people with bipolar disorder, we need these meds to function. I still struggle, even though I take my medication every day, but at least I can function to a certain extent, and that’s more than I used to be capable of. I am grateful for these medications. Please stop abusing them, and giving them a bad name, because when they are NEEDED, they HELP.